I had big plans to give people outside the medical field this dramatic look into the world of the hospital. Throw open the curtain- guys, it’s not like Grey’s Anatomy. (Well, hopefully no one actually thought it was like Grey’s Anatomy. All of the shenanigans in on-call rooms? Guys, hospitals are gross. No one wants to get naked in them.)
Anyway, of course I have gone too long without blogging and now the summer internship seems like a blur. So I’m going to start with a glimpse of what I’m doing now! And then rewind a bit for a bit of curtain-throwing-open based on my summer experience 🙂
The Final Internship
This fall, I am interning with a NICU dietitian for ten weeks! Note that this little subtitle says FINAL internship (!) That’s because once these ten weeks are done, and my master’s paper, which I’ll be doing concurrently, is submitted, I will be a GRADUATE! With a MASTERS DEGREE, aagh!
I’m happy to report that my preceptor is a BOSS. She divides her time between medical nutrition therapy for the tiny NICU babies (lots of critical care stuff), serving as a lactation consultant for mamas with NICU babies, and doing awesome research, including the study that basically made her a STAR, this very cool study about increasing breastfeeding rates in NICU mamas.
Y’all have maybe heard me talk about all my experiences around breastfeeding mamas and breastfeeding promotion. It’s always something I’ve loved. And now it seems like despite my reservations about it (are you qualified to tell someone what to do with their boobs when your boobs haven’t done it themselves?) I have started enough down the pathway to be a lactation consultant that it seems silly to not continue at this point. For example, Tuesday through Thursday of last week I attended the North Carolina Lactation Educator Training Program, receiving hours of lactation-specific education.
Eating taco salad and reading about breast anatomy. As one does.
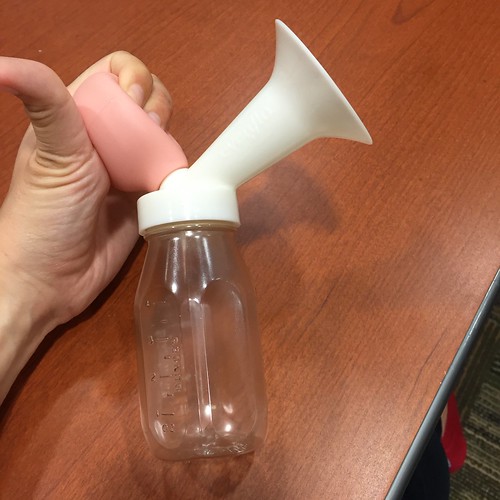
One of my favorite parts of the experience was learning the fairly bizarre history of breast pumps. The original one was essentially a bicycle horn with a suction cup attached (good luck collecting milk; it held about a tablespoon at a time). The next generation was similarly depressing and REALLY difficult to squeeze:
My favorite was this nintendo number here. Eeesh!
This training ended up being fortuitous timing, since my cousin had herself an AWESOME little human in the middle of my training!
Little Chase is already one of my favorite people. My knowledge and skills are still questionable but with (or in spite of?) my help, my cousin is busy feeding this cute little nugget and getting him all big and strong.
I’m excited to see what the remaining ~7 weeks of my fall internship will include. I’m going to be co-authoring (!) a paper my boss is doing on human milk feeding and neurodevelopmental outcomes in premature babies. I’ll be joining the medical team on rounds in the NICU and making recommendations on feeding the little bambinos. And I’m going to continue to try to cultivate my lactation skills to try to attain even 10% of the knowledge of my preceptor (she’s been a lactation consultant for 16 years and is seriously awe-inspiring).
In the meantime, I want to reflect about my prior three months, loving the seaside and getting to know hospital life.
The Summer Internship
My program has its dramas, but I really felt like where they put me this summer was about them knowing me and my academic needs better than I know myself. I feel SO LUCKY to be at the hospital where I was with the team that taught me. My manager was great. The other dietitians were so intentional and generous with their teaching and taught me a ton; they also taught me how to keep learning and were ongoing learners who were constantly trying to increase their own skills and knowledge.
Meanwhile, the hospital was the perfect size for me. My friends who were at GI-NORMOUS teaching hospitals sometimes got a little lost in the crowd, and the professionals there were used to providing educational experiences for medical students and residents that they weren’t really going to go out of their way to provide something for a dietetic intern. My friends at teensy hospitals didn’t get to see many specialties, and anyone with an illness that was super serious (aka super interesting) got transferred out. So my hospital was the SWEET SPOT in the middle of those. I got exposed to so many cool specialties. I got to see someone get a hole punched into their abdomen to insert a feeding tube into their stomach. I got to see the view from a camera down someone’s throat to see how their swallowing worked. I got to see a guy’s SPINE wide open.
Thoughts on specialities
- Pediatrics is awesome. There are no boring cases in pediatrics. This will sound grotesque, but peds cases are fascinating because fundamentally babies and kids are supposed to be healthy. They’re not like adults, whose years of unhealthy decisions have caught up with them and/or their bodies are aging and falling apart. I mean, sometimes babies’ issues are because their parents have made unhealthy decisions. Which is sad.
Some of the other dietitians did not enjoy peds because it’s quite different- you aren’t just planning a diet to support health, you are planning a diet to support GROWTH, in fairly specific numbers (for example, a newborn baby should gain 25-35 grams per kilogram per day, which does actually mean something to me, crazily).
But the best thing about kids is that they can get better! 100% recovery! Really fast! One little girl had come in with appendicitis and by the time I saw her she was eating a plate of approximately 16 strips of bacon. Like a little boss! - Cancer center life is intense. Let’s start with the fact that the top of every patient’s chart it has a spot that says “Goal”. That goal can be “cure” (yay!), “control” (rein in the cancer’s growth as long as you can), or “palliative”. It is sobering as hell how few say “cure” at the top. Nutrition life at a cancer center is *completely* different from everywhere else- most of the time it consists with coming up with ways to cram as many calories as possible into as small a volume as possible. Chemo and radiation jack up your throat and GI tract (“mucositis”= inflammation of all the cells lining all those tubes going through your bodies= pain with every part of the digestive cycle). Your appetite goes away. Your sense of taste is really messed up (a lot of chemo drugs are platinum-based and make everything taste like metal). And cancer cells, vicious buggers that they are, release various molecules that basically cause your lean muscle to melt away. Nutrition is REALLY IMPORTANT and also REALLY CHALLENGING. So we’ll say “Okay, make this milkshake out of heavy cream, peanut butter, and chocolate syrup, and drink it twice a day, and then you won’t have to think about food anymore, deal?” Cancer is also economically as well as physically devastating, which is just another way cancer is super unfair.
- ICUs have almost no direct patient interaction (they tend to be sedated) but are so intellectually satisfying because you’re managing so many things at the same time! Almost everyone’s kidneys start shutting down (organs follow a pretty predictable pattern of crapping out on you- first lungs, then kidneys, then liver) and at that point you have to balance lowering protein- to avoid further stressing the kidney- versus raising protein- because most patients are super catabolic from injuries/inflammation and are burning through their body’s muscle scarily quickly.
Thoughts on doctors:
- Some doctors are amazing. They’re so smart you can’t even believe how they stuff so much knowledge in their brains and manage so many things at once. An amazing moment in womanhood: one day I rounded with a medical team in the surgical/trauma ICU. When we reached one patient, the (female) attending surgeon turned to her (male) resident and very coolly went “You’ll be doing a manual rectal disimpaction on this guy today.”
- Some doctors are awful and it’s frightening how much power they have. In a world where things make sense, increased power in the workplace should correspond with increased accountability in the workplace, right? NOT SO with doctors. If you are ever hospitalized (or your loved one, for that matter), ask to speak with a dietitian on the down low. Or a nurse. They’ll know who are the good doctors and who are the hot messes they wouldn’t let near one of their loved ones in a million years.
- Also if your loved one goes more than 7 days without eating, ask what the dietitian has recommended and followed that. Great doctors do a lot of nutrition research and have a lot of knowledge themselves. They are rare but excellent. The head of the NICU at my hospital over the summer is an example of such a doctor- he has legit written textbooks on neonatal nutrition. Good doctors stay in their lane and defer to the dietitians (nutrition experts) and listen to their judgement. Sucky doctors ignore the dietitians and jack up their patients’ guts. BEWARE OF THEM.
Thoughts on other people in the hospital:
- Wound care are my FAVORITES. Have I mentioned that? Probably. They are just the coolest. They are nurses who have gotten advanced training in taking care of people who have all kinds of scary lines, drains and airways sticking out of their body; all sorts of wounds; all sorts of crazy scary catabolic processes happening. They can take people who have holes in their spines and help make them well! (I saw a guy’s vertebrae, had I mentioned that?! SO RAD.) And they are all just cool, compassionate, interesting, helpful, friendly people. And they respect nutrition!
- Speech and language pathologists (SLPs) are also really cool. Most people know speech therapy as the lady in elementary school who pulls the kid with a lisp out of class for a few hours, but speech therapists should really be called Mouth and Throat and Swallowing and Speaking and Eating experts. They know so much! While healthy people out and about experience food going down the wrong pipe occasionally, aspiration, especially in a hospital setting, is BAD NEWS BEARS. Probably many of you know that pneumonia is often fatal in older adults and aspiration is a real quick way to get there. Knowing that it is or isn’t safe for someone to swallow is absolutely vital information. We also work closely with the SLPs, figuring out what kinds of texture modifications people need.
- Pharmacists are also cool, fun people. I’ve gotten to see them mixing up chemo (!) I’ve seen them making IV nutrition for premature babies (!) I also saw them work on an iron infusion one time, which was a trip- you see the iron in the container and it’s this deep inky blue/purple, and then when they mix the iron with the salts and things in the IV back, it turns RUST colored! I also got to have a really fun conversation about Star Wars with some pharmacists the other week. They’re hilarious. The pharmacy lab is always *freezing*, which is why I can absolutely never be a pharmacist.
Did you not want to end up sick in the hospital? Here are some fairly effective ways to stay out of the hospital:
- Don’t do drugs. Just… don’t do drugs. This summer I was the town with the highest rate of opiate abuse in the nation. Not in my state. Not even in the South. No, this idyllic beachside town has the highest rate of opiate abuse in the ENTIRE UNITED STATES. And sure y’all know doing drugs is bad but… it’s bad. You OD and you end up brain dead. You shoot up and end up with necrotizing fasciitis (FLESH EATING BACTERIA!) in your arm. Or in some other horrible grotesque wound eeesh. Or you get preggers and your kiddo is born and ends up with neonatal abstinence syndrome and has to go on morphine.
- Dude, gastric bypasses are scary. In popular culture they’re viewed as this magical fix that makes you lose a *@#ton of weight, but in reality they JACK YOU UP! Before I started my program I just thought of them as shrinking your stomach for a little bit so you feel full sooner. NOOOO. They cut out a bunch of your stomach but they also cut out a bunch of your small intestine, which means food still goes into your body, but you don’t absorb a lot of the nutrients from it. Calories are the least of that! You miss out on all kinds of essential vitamins and minerals! So it means you MUST supplement EVERY DAY FOR THE REST OF YOUR LIFE or you will end up with potentially life-threatening deficiencies in things like calcium and B12. And God help you if you end up in a phase of life where you are nutritionally at risk and need extra nutrients- like pregnancy! Or fighting cancer! Your system is just not absorbing all you need!
- Know your blood sugar. The next time you go to a doctor, get a fasting blood glucose or an HbA1c (shows your blood sugar over the prior three months or so). If you have prediabetes or diabetes, you want to know it, so you can prevent all the damage excess sugar in your blood can start! I saw so many people who ended up with chronic kidney disease from unmanaged diabetes. CKD is a bitch- you can try to prevent further damage from your kidney from eating a horrifically restrictive diet (do you like high protein foods like meat or milk? Or foods high in potassium like virtually all fruits and vegetables? Say goodbye- all white bread and mayonnaise for you!) Or you can end up on dialysis which is also AWFUL, and you can also get horrible infections from having a needle constantly poking into your skin, letting nasty germies from the outside invade your blood. And then even if your diabetes doesnt result in chronic kidney disease, you can end up with things like blindness! Or limb amputations! These sound like worst case scenarios, except for the fact that I saw them ALL THE TIME this summer.
- Respect your GI tract. Thank God every day that it works correctly. If you start having pain in it, see your PCP sooner than later. It’d be much easier to have someone tell you to cut back on ibuprofen and then get some relief then wait for months and years and be dealing with anemia from your multiple bleeding ulcers.
- Learn CPR! Obvi you can’t use it on yourself but you could use it to save someone else! For reals, I saw a (surprisingly young) person who had gone into sudden cardiac arrest in an athletic endeavor and was saved by someone in the community knowing CPR and using it!
- If you’re over 65 or so, don’t sweat a few extra pounds. It’s a thermal and physical insulator (if you fall you’re less likely to break something). It’s also a nice little reservoir of energy so if you are hospitalized you won’t end up wasting away to nothing. There would be 90something year olds and dummy doctors would put them on diets and we’d be like, “Dude, this person has lived to 94. We should not be putting them on a diet. We should be asking HOW THEY LIVED THEIR LIFE AND HOW CAN WE EMULATE IT.”
Thoughts on life and how my mindset was surrounded by hospital death and gloom all day
- I had my mid-internship site visit with my professor. It went well. Somewhat ridiculously, in the midst of assessing my clinical nutrition assessment skills and offering to troubleshoot any issues with my preceptors, because our program is small and very female, the professor asked, in a motherly tone, how I was sleeping. And I said eh, not great but I wasn’t sure why because the internship wasn’t stressing me out too much. And she was like “Well, Orlando… and that poor little kid at Disney World…” and YEAH THERE’S A LOT OF SADNESS IN THIS WORLD. And a sense of helplessness. I further reflected on this as I walked along the beach one night. I strolled along and thought “Gosh, I’m sad. It’s amazing how one symptom of sleep deprivation for me is just glumness.”And then I went, “Wait. I am in the surgical and trauma ICU this week. I am surrounded by very very sick people this week. Today I had my first patient die (patients have died around me but this was the first time I saw someone one week, did my usual intervention of sending her an Ensure, went off on my merry way, and then came back to her file to discover brain death on it).”
- The patients blur together. You kind of forget that they are people, and that they are sick, and that sickness is a undesirable and unpleasant state of being. You just dig through their file and write down all the abbreviations (ohhhhhh the abbreviations) and pop in their room and ask them the same questions over and over and then every once in awhile there’s this big POP that happens and you snap out of your mode and go “Oh shit this is a person like me except they feel really awful.” Little moments. I went in a room and saw on someone’s white board, that nursing uses, where it said “Pain Goal: 4” and it REALLY depressed me! My pain goal is zero! My day to day pain experience is zero! Or maybe 2 if I have menstrual cramps but those are once a month and relatively undramatic and even a bit satisfying to complain about.
- You think modern medical care is invincible. Probably the doctors go “They’ve got an amiodarone drip! Their heart rate will get back into sinus rhythm and they’ll be fine!” and then we as the dietitians go “We put them on just the right tube feeding! They’re going to tolerate it perfectly and be adequately nourished and get better!” But the body has its limits and sometimes it all goes to &@%.
- We tend to heave a sigh of relief when we’ve seen someone who’s been in the hospital for days/weeks/months and has had intervention upon intervention and pain upon pain and then we see in the note that they’ve gone into palliative care, and we heave a sigh of relief. But it’s easy to forget that yes, pain relief is good and yes, it’s good to end life with dignity but at the same time… it means they’re going to die. Soon. And when you’re surrounded by death you have to reinvent it in the abstract and make it the thing that happens to other people. But it’s not. These patients have to stare down mortality. Plus, even when there’s a big dramatic save, it’s still sad and sucky when you see someone arrive having been independent and leave off to a nursing home where their life is going to be much more limited.
Those are my thoughts! Questions on hospital life?
Also this has nothing to do with the rest of the post but also YOU’RE WELCOME: Lola had her kittens! Not only has she been an incredible mother to them, she is an incredible foster mother! Let me explain: my sister went on Facebook and saw someone had posted in the UNC group that she had found a woeful little kitten all alone in a storm drain! Because my mother was foolish enough to raise her children with compassion, my sister realized that the only logical choice was to hasten a planned trip to Virginia and leave in the middle of the night to deliver this kitten to (hopefully) a loving foster mother.
Because Lola is the BEST CAT IN THE WORLD, and BEST MOTHER IN THE WORLD (well best mother cat; my mother is the best mother human, who herself is doing a VERY generous thing fostering Lola!) she adopted the little kiddo like he was her own.
One of these kittens is not like the others!
But Lola does not mind. Little kitten can still join the snuggle box.

The little guy is a little older and thus a little more playful than the other kittens. My sister has named him Clovis. Clovis enjoys biting and pouncing.

He also loves his mommy, as do his adopted brothers and sisters.

With all the breastfeeding promotion work I am now doing, I am definitely going to find a good place to use this picture.




Good post! Can I share? I developed HFMD from baby Alexandra. Was my body low on something that only I got it from her? now, finger nails are coming off and skin is peeling.
b
>
I am so sorry, that sounds awful! I’d definitely talk to your primary care provider about it- I don’t know enough about hand foot and mouth and haven’t ever seen anyone hospitalized for it. I wish I had something to recommend!